Tuberculosis (TB) is a bacterial infection, that mostly occurs in the lungs, spread by droplets in the air released when an infected person coughs or sneezes. The mycobacteria that cause TB are clever at evading the body’s immune system and many people carry the disease without realising they are infected, this is called Latent TBI. About 5 percent of patients are at risk of developing TB.
Incipient TB infection
Following initial contact with M.Tuberculosis (Mtb) about 5 per cent of patients progress rapidly to active tuberculosis (TB) disease.
Although some are able to eliminate the disease through innate or acquired (vaccination) immune response, the majority will develop a latent reaction, becoming carriers of the disease.
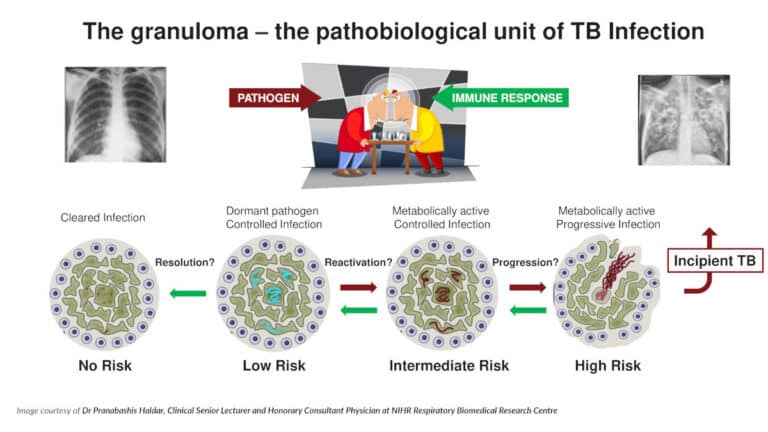
It is thought that Mtb will lay dormant in the body controlled by white blood cells within a granuloma, the disease may be triggered at some time in the future if the person becomes stressed, malnourished or immunocompromised.
Control of the disease therefore lies in determining which of these patients with latent TB are likely to progress to full disease status – this group is known as having Incipient TBI.
The pathway is complex and impacted by:
- The health status of the host – those with HIV and diabetes, malnourished or under stress are more likely to develop disease
- Genotype and phenotype of the strain of Mtb – some strains are more virulent
- Genotype of the host – some people have improved innate immune response
- Access to treatment – TB is preventable with medication
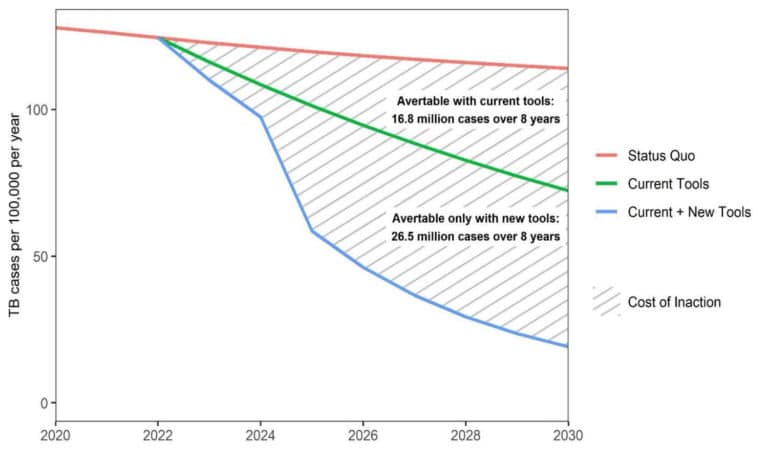
If those with Incipient TBI could be easily detected, then appropriate treatment could be given preventing progression to full disease. Targeting effort in this way would be cost-effective and reduce the risk of resistance to the medication.
Detecting incipient TB
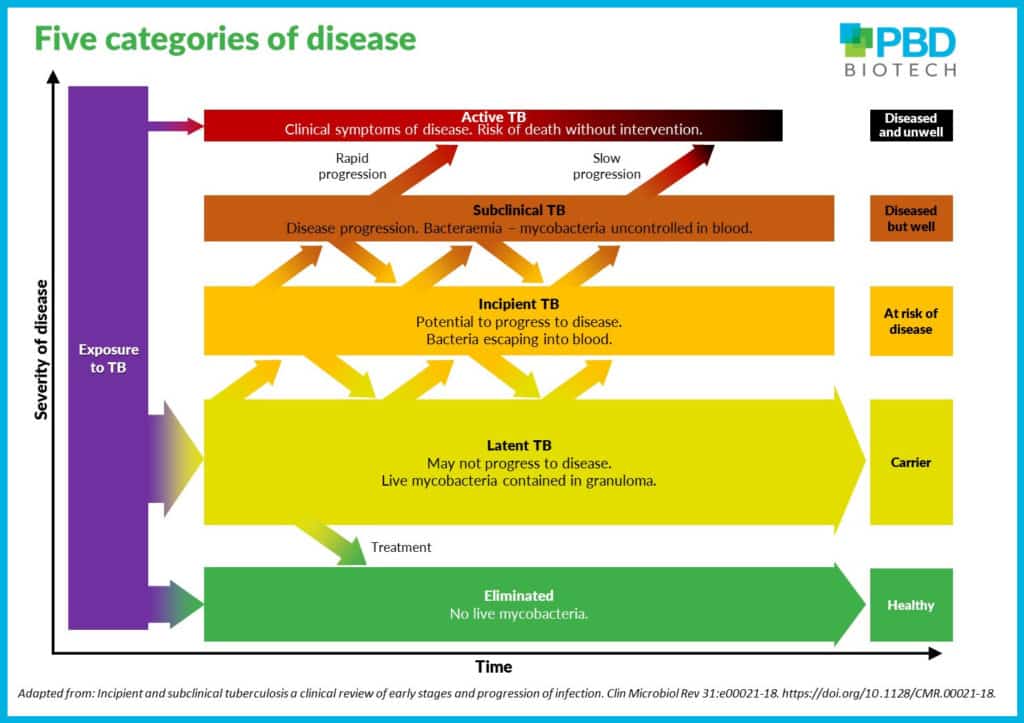
The five categories of TB infection in the spectrum of TB pathogenesis, were identified by researchers Paul K Drain et al (2018). They were among the first to identify an incipient and subclinical stage and this is supported by PET-CT scans that showed lesions detectable in asymptomatic individuals correlate with the onset of subclinical TB disease and with progression toward active disease.
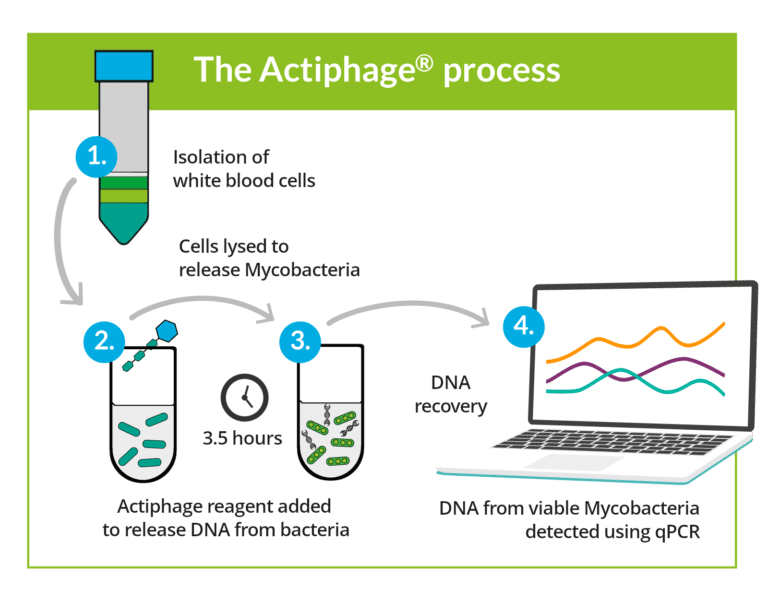
Researchers at Leicester used Actiphage to test the hypothesis that Mtb detectable in blood soon after infection associates with incipient TBI as it indicates that the infection is no longer being controlled.
It was the first study to successfully isolate Mtb in the blood and to use this to distinguish between latent TBI and incipient TBI.
Five categories in the spectrum of TB pathogenesis
- Eliminated – no viable mycobacteria, immunological evidence of infection.
An individual with prior exposure to M.Tuberculosis who has cleared the infection through innate or acquired immune response, or been cured through medication. Skin tests and IGRA will show positive, by detecting dead mycobacteria and immune response to contact with Mtb. - Latent TB – positive tuberculin skin test reaction, no clinical or radiological evidence of active disease.
The immune system is able to fight the bacteria and stop them growing by containing them in granuloma. Progression to TB disease is not expected to occur in near future if the person is not immune compromised. - Incipient TB – viable mycobacteria, no clinical symptoms.
Infection with viable mycobacteria that is likely to progress to disease in absence of intervention. Scans using FDG/PET combined with PET/CT have identified lesions in asymptomatic individuals that correlate with subclinical disease, indicating those most likely to develop active disease.
Evidence from Actiphage show that mycobacteria are escaping from granuloma and present in blood. This is found to correlate with FDG/PET scans. - Subclinical – viable mycobacteria, radiological abnormalities.
Disease state that does not have visible symptoms but demonstrates radiological abnormalities. Significant bacteraemia with uncontrolled mycobacteria in the blood, detectable with Actiphage. - Active TB – viable mycobacteria, radiological abnormalities. Active disease with radiological abnormalities and clinical symptoms that will usually include:
- loss of appetite and weight
- persistent cough
- bring up phlegm; they may also cough up blood if a blood vessel becomes damaged
- unusual tiredness
- fever – that can result in heavy night sweats.